A beginner’s guide to alexithymia
By Jerrod Brown
November 2022

Alexithymia is a complex, subclinical phenomenon characterized by cognitive-affective functioning impairments that can affect as many as 10% of the general population. Typically, individuals with alexithymia struggle to recognize, identify and describe their feelings. This often includes trouble discerning between emotions and physiological sensations. Because alexithymia is a known risk factor for a wide range of psychological and physical health problems, this psychological construct has significant implications for professionals working in the field of mental health. In fact, the failure to accurately identify the presence of alexithymia can significantly impact the intake, screening, goal-planning and therapeutic processes. Therefore, mental health professionals should become familiar with the wide array of disorders, traits and experiences often associated with elevated rates of alexithymia.
Unfortunately, many mental health professionals lack the necessary training and expertise to accurately identify and effectively treat the unique and complex symptoms of alexithymia. A strong contributor to this predicament is the lack of training and educational programs that offer workshops and coursework dedicated to this important and complex topic. The goal of this article is to provide mental health professionals with a basic introduction to alexithymia by highlighting information in four essential areas: (a) symptoms and red-flag indicators, (b) diagnostic comorbidity, (c) screening and assessment and (d) intervention and treatment considerations.
Symptoms and red-flag indicators
Symptoms of alexithymia can vary from person to person and are often influenced by many neurological, biological and psychosocial factors.
The cognitive factors associated with alexithymia can include:
- Deficits in the regulation of thoughts, emotions and bodily processes
- Difficulty with introspection
- Inhibition and impulsivity issues
- Limited imagination and fantasy life
- Constricted patterns of thought
- Reliance on concrete thinking almost to the exclusion of symbolic thinking
- The affective factors associated with alexithymia can include:
- Blunted or limited personal experience of emotions
- Difficulty identifying and describing emotions
- Emotion dysregulation
- Failure to identify the causes of personal feelings
- Inability to seek and use support systems to help with emotional problems
- Limited use and understanding of verbal and nonverbal emotional cues
- Poor emotional awareness
- Emotional avoidance and suppression
- Difficulty distinguishing between emotions (e.g., telling the difference between anxiety and anger)
- Weak affective theory of mind
- The social factors associated with alexithymia can include:
- Interpersonal communication characterized by coldness, flatness and a lack of emotion
- Lack of empathy
- Loneliness
- Nonassertiveness
- Perspective-taking deficits
- Social conformity
- Verbal and nonverbal communication deficits
- Weak social attachments
- The physiology factors associated with alexithymia can include:
- Physical sensitivity to the experience of different sensations
- Tendency to mistake affective responses as physiological experiences or dysfunctions
Diagnostic comorbidity
Alexithymia often co-occurs with a diverse array of psychiatric, trauma-based, neurocognitive, neurodevelopmental and substance use disorders, so it is likely that mental health professionals provide services to clients impacted by alexithymia on a regular basis. In particular, individuals with alexithymia are quite prone, but not limited, to presenting with another disorder that features affective symptoms. It is important to note that alexithymia can be viewed as a risk factor for psychopathology as well as other conditions. The following highlights some mental health conditions often associated with alexithymia.
Substance use and other addictive disorders. The prevalence rates of alexithymia are higher among individuals with substance use and addictive problems than the general population. In addition, individuals with alexithymia appear to be at risk for more severe alcohol-related problems than those without alexithymia. This has led some researchers to posit that alexithymia could place a person at risk for alcohol use problems. Failure to consider the role of alexithymia in alcohol use could undermine the effectiveness of any interventions.
Stress-related disorders. Research has consistently linked alexithymia to physiological stress markers as well as stress-related disorders. For instance, individuals with alexithymia often exhibit elevated levels of chronic stress on measures of cortisol awakening response and cortisol secretion during the dexamethasone suppression test. Other evidence includes increases in inflammation and atypical immune responses, which could be consequences of prolonged exposure to stress.
Posttraumatic stress disorder. Posttraumatic stress disorder (PTSD) is a condition characterized by heightened reactions, anxiety, intrusive memories and nightmares, and other-related symptoms. The onset of PTSD is precipitated by exposure to a traumatic event (e.g., violence, accidents, natural disasters). Some of the same traumatic experiences that lead to PTSD could also contribute to the development of alexithymia. As a result, mental health professionals are encouraged to screen for alexithymia in clients presenting with PTSD.
Insecure attachment. Research has found higher rates of alexithymia among people with insecure attachment patterns compared to people with secure attachment patterns. Insecure attachment patterns may also cause the impacted individual to experience trust issues, fears of abandonment, general discomfort and decreased coping abilities. And both insecure attachment patterns and alexithymia have been linked to increases in emotional and behavioral problems. Therefore, attachment-based therapists are encouraged to become informed about alexithymia.
Traumatic brain injury. Traumatic brain injury is temporary or permanent brain damage caused by a blow or some other wound to the head. Common symptoms of traumatic brain injuries include impulsivity, aggression, emotion dysregulation and poor coping skills when under duress. Research shows that many people who suffer from a traumatic brain injury also experience alexithymia.
Neurodevelopmental disorders. Alexithymia has also been found to be elevated among people diagnosed with neurodevelopmental disorders, including attention-deficit/hyperactivity disorder, autism spectrum disorder, fetal alcohol spectrum disorder, and intellectual and developmental disability. Routine screening for alexithymia among people diagnosed with a neurodevelopmental disorder may lead to improved treatment outcomes.
Hypothalamic-pituitary-adrenal axis dysfunction. The hypothalamic-pituitary-adrenal (HPA) axis may play a role in alexithymia. This system is responsible for regulating stress responses and ensuring the body adjusts to evolving environmental conditions. Exposure to stressful situations can elicit chronic hyperactivity of the HPA axis. In such instances, a person becomes at risk for stress-related physical and mental health problems. Because of the potential connection, I recommend counselors also become informed about the HPA axis when learning about alexithymia.
Somatic symptoms. Individuals with alexithymia tend to score higher on measures of physical distress than the general population. These physiological differences could help explain the higher prevalence of anxiety and depression symptoms among those with alexithymia. During times of distress, people with alexithymia may experience and complain more about psychosomatic-based symptoms.
Dissociative tendencies. Dissociation occurs when there is a disconnection among a person’s cognitions, emotions and actions. The presence of dissociation could play a role in the emergence of alexithymia or vice versa. This is particularly salient in people who have experienced trauma such as neglect and abuse. In such cases, the development of dissociation and alexithymia could serve as an adaptive response that prevents a person from being overwhelmed.
Sleep disturbances. Individuals with alexithymia often report comorbid sleep problems. These can include difficulties with staying awake or falling and staying asleep. Emotional problems that are similar to alexithymia have also been observed among individuals experiencing sleep deprivation.
Language problems. Individuals with alexithymia often struggle with verbally expressing their own emotions. In addition, individuals with alexithymia have trouble comprehending the verbal communications of other people. Therefore, problems with language processing could be an important causal influence on the development of alexithymia.
Executive dysfunction. Individuals with alexithymia commonly exhibit deficits in executive function, which is a set of cognitive, affective and behavioral skills that enable a person to plan and perform specific tasks. In particular, cognitive flexibility, inhibition and working memory are often described as the primary aspects of executive function. It is important to note, however, that many other constructs fall under the umbrella of executive function. The symptoms of alexithymia and deficits in executive function may be exacerbated by various forms of extreme stress and trauma. When this occurs, it can significantly impede goal achievement and adaptive functioning.
Immune function dysregulation. A growing number of studies have reported an association between alexithymia and immune system dysregulation. The same stressors that cause alexithymia could also alter how the immune system functions. A grave consequence of immune system dysregulation includes proneness to a diverse array of psychosomatic illnesses. Encouraging the client with alexithymia to maintain regular contact with their health care provider is warranted.
Emotional regulation deficits. Individuals with alexithymia often present with emotional dysregulation issues. For example, individuals with alexithymia usually struggle to express or understand their feelings and the feelings of others. As a result, many mistake the symptoms of alexithymia as a lack of empathy. Consequences of emotional dysregulation include difficulties with establishing and maintaining relationships across the life span. In some instances, this could lead to a breakdown in the therapeutic alliance.
Worry and rumination. Individuals with alexithymia typically experience high levels of worry and rumination. Worry is generally distinguished by fears of danger, whereas rumination is characterized by thoughts about loss and failure. These repetitive cognitive processes are common in internalizing disorders (e.g., anxiety, depression).
Deliberate self-harm. Empirically based research has found an association between alexithymia and a history of substance abuse and deliberate self-harm. Such self-injurious behaviors could be an attempt to cope with emotional dysregulation, which is frequently exacerbated by alexithymia.
Suicide risk. Alexithymia could serve as a risk factor for suicidal behaviors. Individuals with alexithymia are prone to depression, anxiety and other affective problems, all of which are also predictors for suicidal behaviors.
Screening and assessment
Clinicians should carefully screen for alexithymia prior to the development of mental health and substance use treatment plans. The Toronto Alexithymia Scale (TAS-20) is one instrument counselors can use to screen for alexithymia. The TAS-20, which is commonly used in neuroscience studies, is a 20-item, self-report questionnaire that measures skills in the areas of emotion recognition, emotion description and perspective-taking. Several empirically based articles have been published pertaining to the efficacy of the TAS-20.
When screening, clinicians should watch for increased symptom reporting. Individuals with alexithymia are prone to confusing emotions and feelings for physiological problems with their bodies. In turn, this group is disproportionately likely to overreport and seek medical care for physiological problems. This is another example of maladaptive coping in the context of alexithymia.
As mentioned in the previous section, individuals with elevated stress and anxiety, burnout, or a history of trauma are predisposed to alexithymia. Therefore, systematic screening and assessment for alexithymia is encouraged in these groups. Trauma-informed counselors would also benefit from learning about alexithymia.
Emotional numbing and emotional suppression are two other areas that mental health providers should consider during the intake and treatment planning process. Emotional numbing is the affective process of minimizing or eliminating the experience of feelings. Like alexithymia, this could be viewed as a temporary coping strategy that is deployed to protect against the consequences of trauma. And emotional suppression is a common way that individuals with alexithymia regulate their feelings. This may be traced back to difficulties in recognizing and understanding emotions that characterize alexithymia.
It is also critical that mental health professionals obtain information from collateral informants when screening for alexithymia. In many instances, the client may lack insight into their own symptoms, which renders self-reported information as insufficient. So conferring with family members, friends and co-workers can help illuminate the nature of the client’s symptoms and their impact on global functioning. In addition, consulting with any other professionals that work with the client can be informative.
Intervention and treatment considerations
Individuals with alexithymia typically have worse mental health treatment outcomes than those without alexithymia. In an effort to address this quandary, research has focused on identifying interventions that help improve outcomes for individuals with alexithymia. This section highlights potential considerations that mental health professionals should make when treating alexithymia.
The symptoms of alexithymia likely undermine the development of therapeutic alliances with mental health professionals. Specifically, difficulties with recognizing and describing affective experiences as well as perspective-taking make it difficult to develop interpersonal closeness with others.
In addition to limiting the development of the therapeutic alliance, alexithymia could be associated with poor treatment engagement. In combination, these suboptimal outcomes in the therapeutic process contribute to an increased likelihood of negative short- and long-term treatment outcomes in individuals with alexithymia.
The difficulties that alexithymia presents in terms of the therapeutic alliance and treatment engagement are particularly salient in substance use treatment settings. Clients with alexithymia may be dependent on the use of substances to cope with the affective symptoms of their condition. The failure to account for and address alexithymia during the therapeutic process decreases the likelihood of good treatment prognosis.
Individuals with alexithymia are also prone to poor treatment attendance and adherence, which can be expected among clients with poor treatment engagement. Thus, failure to complete treatment programs and relapses are common in clients with alexithymia.
The research literature on the treatment of alexithymia has grown in recent decades, and there is now a substantive list of interventions worth considering when treating clients with alexithymia (see table below). Psychoeducation offers one promising treatment option for clients with alexithymia. A limited but growing body of research indicates that supportive and psychoeducational approaches to therapy may be effective in treating alexithymia. Interpretive approaches to therapy, however, appear to be less effective with this population.
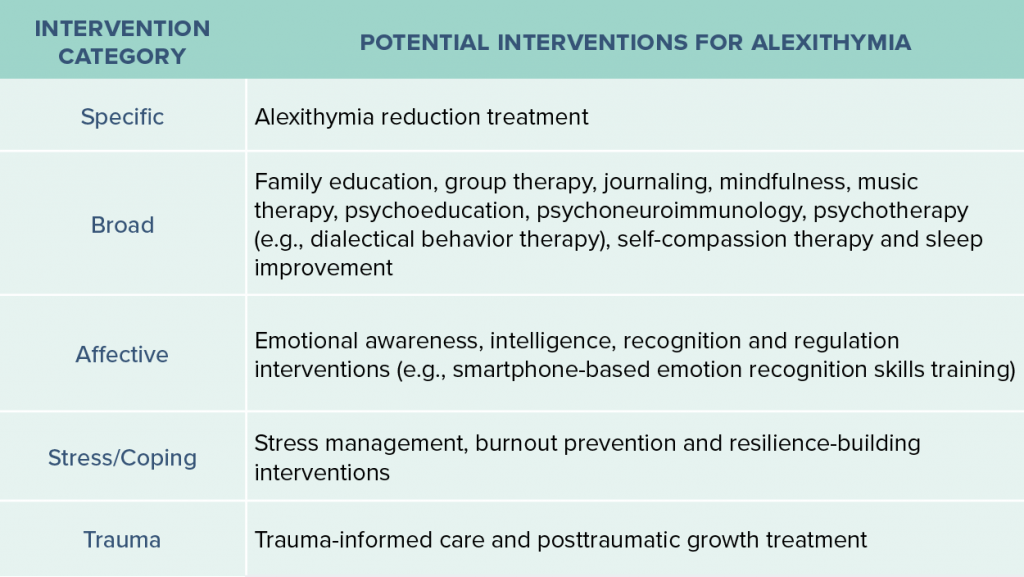
Mindfulness training may also be a critical component to incorporate in the treatment of alexithymia. For instance, mindfulness-based training has been linked to increased emotional effectiveness. So using mindfulness-based approaches may result in improved emotional awareness among clients experiencing alexithymia.
Music therapy also holds promise as an intervention for clients with alexithymia. This therapeutic approach is particularly well suited for clients who struggle to describe thoughts and feelings with words. Thus, clients with alexithymia may find it easier to express their emotions in music therapy.
Individuals with alexithymia generally struggle with emotional clarity, which is the ability to recognize and understand the causes of one’s emotions. Development of emotional clarity could help a client with alexithymia not only benefit from treatment but also protect against victimization in their personal life.
Clinicians can also help clients with stress management. A common risk factor for alexithymia is the experience of extreme stress. It is unsurprising, then, that individuals with alexithymia often struggle with stress management. Thus, the development of stress management skills remains a critical target in any intervention for clients with alexithymia.
Conclusion
Alexithymia is a complex and important topic all mental health clinicians need to know. Since elevated rates of alexithymia are found in a host of trauma-based, substance use, neuropsychiatric, neurocognitive and neurodevelopmental disorders, it is likely that mental health professionals will encounter clients impacted by this subclinical, cognitive-affective deficit on a regular basis. Unfortunately, in my experience, few professionals working in the field of mental health have received sufficient education and training pertaining to the topic of alexithymia.
I strongly encourage all helping professionals to become informed about alexithymia. Here are three ways counselors can begin this process:
- Seek professional consultation from recognized alexithymia experts.
- Review key journals in the field on a regular basis to stay abreast of the latest peer-reviewed research on alexithymia.
- Continue to seek education and training on the best ways to screen for alexithymia and the best intervention techniques to use with clients who struggle to identify and describe their emotions.
Important facts about alexithymia
Here are some important reminders mental health professionals need to consider when learning about the topic of alexithymia:
- Alexithymia is a threat to emotional, social, and physical health and well-being.
- Alexithymia is not considered a mental health disorder and is mentioned only once in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders.
- Alexithymia is a trait found elevated among people diagnosed with neuropsychiatric, neurocognitive, neurodevelopmental, trauma and stressor, and substance use disorders.
- Numerous empirically based articles have been published on the topic of alexithymia.
- Alexithymia can amplify stress and its impact on emotional, social, behavioral and physical health.
- Clients with alexithymia have difficulty understanding, processing, recognizing and describing emotions.
- During times of increased stress, worry and conflict, people impacted by alexithymia frequently experience an increase in psychosomatic-based symptoms.
- Alexithymia can impede the therapeutic alliance, especially when mental health providers lack an awareness and understanding of this topic.
- When becoming trauma informed, it is also important to become alexithymia informed.
- Professionals are strongly encouraged to seek out additional training and consult with experts to better understand the implications of alexithymia within mental health and substance use treatment settings.
- Academic-based institutions and continuing education training programs are encouraged to offer curriculum and workshops pertaining to the mental health implications of alexithymia.
****
Jerrod Brown is an associate professor, program director and lead developer for the master’s degree in human services with an emphasis in forensic behavioral health and in trauma, resilience and self-care strategies for Concordia University in St. Paul, Minnesota. He has also been employed with Pathways Counseling Center in St. Paul for the past 19 years. Contact him at Jerrod01234Brown@live.com.
Counseling Today reviews unsolicited articles written by American Counseling Association members. To access writing guidelines and tips for having an article accepted for publication, visit ct.counseling.org/feedback.
**** Opinions expressed and statements made in articles appearing on CT Online should not be assumed to represent the opinions of the editors or policies of the American Counseling Association.

