Suicide affects all ages and groups
Throughout the month of September, mental health organizations around the country recognize Suicide Prevention Month. However, working together to develop our collective understanding and awareness of suicide in order to prevent it is something we need to be doing every day. Talking to a counselor about any questions you have about how to help support others or how to get help for yourself is a great place to start.
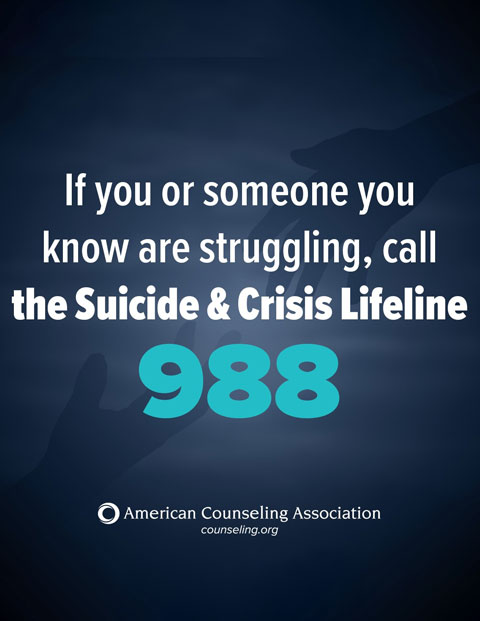
Call or Text 988
The 988 Lifeline is a suicide and crisis lifeline, which uses a network of 200+ local crisis centers to connect people with 24/7 free and confidential support.
SUICIDE RESOURCESCrisis Center Information
In addition to the 988 Suicide and Crisis Lifeline, the following resources are available if you, or someone you know, need help:
- Veterans Crisis Line: 1-800-273-8255, press Option 1
- Trans Lifeline: 1-877-565-8860 (U.S.) or 1-877-330-6366 (Canada) The Trans Lifeline’s Hotline is a peer-support service for trans and questioning individuals in crisis. All operators are trans-identified.
- Trevor Lifeline: 1-866-488-7386 The only national 24/7 crisis intervention and suicide prevention lifeline for LGBTQ young people under 25.
- TrevorText: A free, confidential, secure service in which LGBTQ young people can text a trained Trevor counselor for support and crisis intervention, available Monday–Friday from 3–10pm ET / Noon–7pm PT by texting START to 678678.
- Crisis Text Line: Crisis Text Line is a crisis-intervention hotline that conducts conversations exclusively by text message. Trained crisis counselors are available 24 hours a day.
- Disaster Distress Helpline: 1-800-985-5990 - SAMHSA’s Disaster Distress Helpline provides 24/7 crisis counseling to people experiencing emotional distress related to natural or human-caused disasters.
- Mental Health - Warm Lines: Warm lines are confidential, peer-run listening lines staffed by people who have experienced mental health conditions themselves.

Advocacy
How Counselors Can Advocate during Suicide Prevention Month
Related Articles from Counseling Today
General Public Resources from the Counseling Corner
How Should We Be Talking About Men's Mental Health?
/mens-mental-health-month.png?sfvrsn=ff74f976_4)
June is National Men’s Health Month. And while men’s mental health is certainly acknowledged as a key component of their overall health and well-being, its importance is often overshadowed by concerns about everything from conditions like high blood pressure and heart disease to the threat of prostate cancer or Alzheimer's disease as men continue to age.
The numbers behind men’s health
There’s a long list of statistics all pointing to facts like men are less likely to take care of themselves than woman, men will wait longer to seek medical help for any health issues or concerns and men are more likely to develop substance use disorders. According to the National Center for Health Statistics, the life expectancy for males at birth dropped from 76.3 years in 2019 to 75.1 in 2020, further increasing the life expectancy gap between males and females (80.5 years in 2020) to 5.4 years.
And when we shift that statistical focus to men’s mental health, the picture isn’t much brighter. According to the American Foundation for Suicide Prevention, men died by suicide 3.6 times more often than women in 2019. Mental Health America notes that one in five men develop alcohol dependency during their lifetimes and gay and bisexual men are more likely to have higher rates of substance abuse than heterosexual men.
Among men between the ages of 18 and 44 who had daily feelings of anxiety or depression, non-Hispanic Black men and Hispanic men were less likely than non-Hispanic White men to have used mental health treatments. And all these numbers are fueled by archaically gendered stereotypes that reinforce beliefs that men should be able to control their emotions and feelings and that talking about those things openly is taboo if not downright “unmanly.”
Choosing contemporary mental health talk over outdated gender stereotypes
The reality is that if we want to pursue a substantive conversation about “men’s health,” thoughtful discussion about men’s mental health should be front and center. And if we want to make that discussion a productive one, we need to embrace compassionate, contemporary and rationale ways of talking about mental health that defy outdated, gender-based perspectives. And, slowly but surely, that’s exactly what’s happening.
Encompassing some older efforts as well as some new, there is a growing collection of initiatives and advocacy campaigns designed to unravel the stigma surrounding men’s mental health needs and reframe the conversation in ways that speak to individuals in need.
Pursuing effective mental health campaigns for men
The Man Therapy campaign cut right through the stigma duct tape with clever marketing and engagement efforts with reminders like, “You can’t fix your mental health with duct tape,” and “It’s ok to cry, even when it’s not about sports.” One of the most clever and critical factors underscoring Man Therapy is understanding why certain groups of people, in this case middle-aged working men, “check out” anytime they hear the topic of mental health brought up and finding more effective strategies for connecting with them.
Therapy for Black Men and Men Thrive are two incredible examples of efforts to acknowledge the unique mental health challenges faced by Black men. From providing targeted resources and carefully curated communities of support to calling out the “generational toxic stress, depression, and anxiety” that prevent Black men from thriving, these projects call out directly the combined effects of toxic masculinity and systemic racism and champion a new mental health movement that celebrates and centers Black men.
And there are organizations like Movember that have been working for the last two decades to fund projects focused on challenging the status quo around men’s health and “transforming the way health services reach and support men,” including services focused on mental health.
If we want to support overall health and well-being for any group or individual, we have to acknowledge two fundamental notions: 1) Mental health is an essential component of overall health and needs to be centered in the conversation, and 2) If we want men, and anybody else for that matter, to engage in a conversation about mental health, we need to understand what speaks to them (and what doesn’t) and why, and do everything we can to facilitate that conversation.